Lately, I’ve been thinking about genetic testing for cancer.
Have you ever had that feeling that certain health issues might be lurking around the corner? That’s exactly where I found myself not too long ago. As I entered my 50s, the routine check-ups turned into a regular series of deeper screenings, ultrasounds, biopsies, and specialist visits.
It’s not that I’m unhealthy – I take care by eating organic, loading up on fruits and veggies, and preferring fish over red meat. But then, based on my family history, my OBGYN referred me for genetic cancer screening and evaluation at a high-risk clinic that provides personalized early detection and personalized care programs for people with cancer predisposition genes.
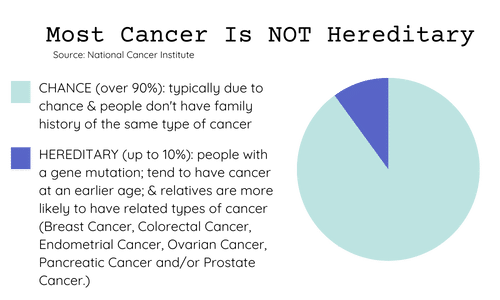
Prevalence of Hereditary Cancer
Conversation with Genetic Counselor
This was all new to me and I was curious about how it all works. So I took the first step and had a call with a Licensed Certified Genetic Counselor. She explained the process to me while she asked me numerous questions about my health and my family history of cancer. She also answered all of my questions as she evaluated whether I met the national guidelines for preventative genetic screening and the corresponding high-risk programs. My program partners with the NCI-designated Comprehensive Cancer Center in my state providing access to advanced cancer treatments and related clinical trials. (See below for more information.)
The option of genetic testing came up – using a swab just like those ancestry tests. Yet, my privacy concerns kept me at bay. It’s not just about my data out there. I’ve supported medical research in the past. It’s about the whole chain reaction of companies owning my genetic information and possibly using it in ways other than for medical research — selling it. My privacy radar blipped intensely.
This was all new to me and I was curious about how it all works. So I took the first step and had a call with a Licensed Certified Genetic Counselor. She explained the process to me while she asked me numerous questions about my health and my family history of cancer. She also answered all of my questions as she evaluated whether I met the national guidelines for preventative genetic testing and the corresponding high-risk programs. My program partners with the NCI-designated Comprehensive Cancer Center in my state providing access to advanced cancer treatments and related clinical trials. (See below for more information.)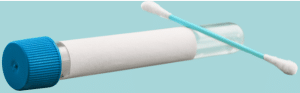
The option of DNA testing came up – using a swab just like those ancestry tests. Yet, my privacy concerns kept me at bay. It’s not just about my data out there. I’ve supported medical research in the past. It’s about the whole chain reaction of companies owning my genetic information and possibly using it for ways other than medical research — selling it. My privacy radar blipped intensely.
The mechanics of the genetic cancer test were simple – a swab of saliva sent to a lab or a blood draw. The counselor explained that, if I prefer not to have my blood drawn, the DNA sample could be collected at home using the Empower™ hereditary cancer test by natera. The lab would share my results with my doctor, and my insurance company, and then de-identify them for use in research and development. That’s what gave me pause.
Yes, they promise confidentiality, but having observed data privacy challenges in the tech industry was enough to cause concern about the privacy of the genetic research data across all of these companies. That’s a territory where sustained privacy feels both essential and blurry.
Family History and Family Concerns
Following the genetic counseling, my family history weighed heavy on my mind. If I found out I carried genetic mutations, what then? How would it affect not just me but also my sister, who shares similar DNA? And my children? These were knots I wasn’t ready to unravel just yet.
Big Question Remained
The big question also echoed: Would knowing change anything for me? I dwelled on my grandmother’s battle with cancer, the treatments, the struggle, and yet, in the end, her passing wasn’t solely attributed to cancer.
Then, there’s my sister. Would this information affect her? Would she even want to know? I felt compelled to consider her stance in all of this.
Insurance and Privacy Concerns
Insurance was another minefield. Laws might say it can’t be held against me, but stories of coverage denials and uncertainties lurked in my thoughts. It’s a gamble on the unknown. Is genetic predisposition to breast or colon cancer a pre-existing condition? Will it be a reason to deny a future life insurance policy or long-term care coverage? Will the genetic test results trigger flags for my current health insurance provider?
The idea of lifetime support from the genetic program coordinators was appealing. But the potential toll on finances and emotions felt overwhelming.
- What would I pay vs. what insurance covers?
- How would I access the information?
- What personal information would my insurance company have?
These questions lingered, unanswered.
More Questions
Amid this whirlwind of doubts, there was a revelation – less than 5% of people tested have markers for the cancers screened. It made me ponder:
- Would I be among them? Then what?
- Would I be faced with decisions on potentially radical prevention options?
- Is the anxiety worth it for such a low probability?
My Answer for Now
Eventually, after much contemplation, I chose not to proceed with the genetic cancer test. Not because I don’t care about my health or because I don’t value the importance of early detection, but because the uncertainties outweighed the urge to know.
The saying may be true. Ignorance is bliss!
I feel healthy. As I continue to age, I won’t always have that luxury. So I will plan for health — not for whatever future challenges the crystal ball of my DNA may reveal.
This decision may change in the future. My circumstances might evolve, but I’ve chosen this path for now. Perhaps my journey might resonate with you if you find yourself at this crossroads. Remember, it’s not a matter of not caring, but sometimes being courageous means choosing not to know.
Resources to Learn More about Hereditary Cancer
FORCE is a 25-year-old non-profit organization, rich with resources for people facing hereditary cancer.
56 NCI-Designated Comprehensive Cancer Centers in 32 states provide programs, including genetic counseling for people in families with inherited gene mutations.
NSGC Member Directory of 3,300+ genetic counselors in North America.
Genetic testing is a personal decision and there are many views about the risks and benefits. Here read how Nancy McLernon views genetic testing.
Share this post:
Author
-
Christy is a wife, mother of twin teenagers, a 3x CMO, an advisor and mentor who lives in the Seattle area. She finds joy in the everyday magic of nature and wildlife and loves to travel, cook, garden, and spend time with family and friends.
View all posts